Parkinson’s Disease
 Overview of Parkinson’s Disease (PD)
Overview of Parkinson’s Disease (PD)- Parkinson’s disease is due to degeneration in a part of the mid-brain called “substantia nigra”, resulting in insufficient production of “dopamine”, which is a chemical responsible for transmitting signals in the nervous system.
- The decrease in the amount of “dopamine” in the brain directly affects the control of motor activities, leading to limb stiffness and slowness of movements of the patients.
- The cause remains largely unknown. Although there is no cure, treatment options vary and include medications and surgery.
- Besides medical treatment provided by doctors, evidence showed that exercise with education provided to patients and their carer can help them improve their physical ability and cope with the daily living.
Typical Clinical features in Parkinson’s disease:
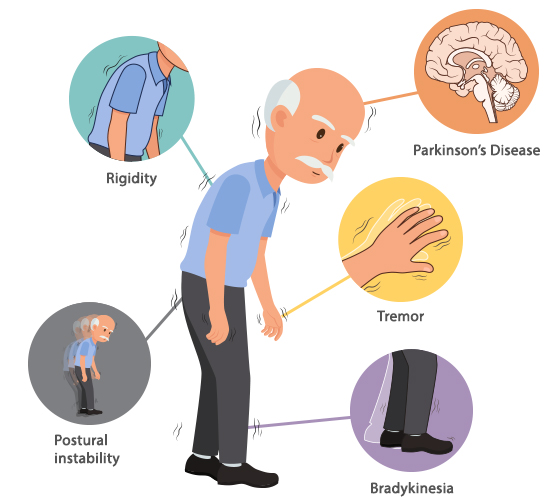
- Slow in speed, small in amplitude (bradykinesia)
- Tremor of arm, hand or leg.
- Rigidity of body, arm or leg
- Loss of postural control means cannot regain balance when fall down.
Hoehn and Yahr (HY scale)
- The Hoehn and Yahr Scale is used to measure how Parkinson’s symptoms progress and the level of disability.
- Originally published in 1967 in the journal Neurology by Margaret Hoehn and Melvin Yahr.
- It included stages 1 to 5

Physiotherapy treatment for patients with PD
- Physiotherapy aims to keep body moving safely and independently and help patient managing PD symptoms and maximise the quality of life
- The key aims of physiotherapy in Parkinson's are:
- to maintain and improve functional ability and independence
- to correct and improve posture and balance
- to minimise the risk of falls
- to allow strength and flexibility to be maintained
- to enhance daily activities (getting in and out of bed, rising from a chair)
- to maintain a safe walking pattern (with or without mobility aids)
- if freezing is evident, coping strategies such as auditory or visual cues may be taught
- to improve manual activities (reaching and grasping)
- to maintain respiratory function through breathing exercises
- to teach relaxation techniques
- to educate carers
Recommendations on exercise for patient with PD
| ENDURANCE |
|
| STRENGTH |
|
| FLEXIBILITY |
|
| BALANCE |
|
Key Elements of Physiotherapy treatment for patients with PD
Cardiovascular training
Moderate intensity exercise 30 mins, 5 times per week


Movement Strategy
Horizontal lines on the floor are visual cues to help PD patient to start walking if they have freeze of gait. Laser cane emits a red line on floor is another type of visual cue.



Strength Training
Using bands 、weights, boxing or machine to train big muscle group, 2-3 non-consecutive day, 8-12 repetitions per set


Balance
2-3 days per week for 20-30 mins, challenge on balance, agility and coordination

Stretching
At least 2-3 days per week, hold for 30-60 seconds


Hydrotherapy

Postural Correction


